Welcome,
Getting Someone In and Out of Bed Safely can be difficult! Here are some bed mobility techniques to make getting in and out of bed easier. I encourage you to watch the video and continue to read for more information as well as an opportunity to ask any questions!
Bed Mobility Training…Get Someone In & Out of Bed Easier
It’s Too Hard…It Will Hurt…I Don’t Want To…
Sounds like the excuses for not exercising, but these are the excuses I get from most patients when I approach them with the task of getting out of bed. Weakness, muscle atrophy from inactivity, and other very serious problems can occur when someone stays in bed! Bed sores, blood clots, and an increased risk for choking are just a few reasons for patients to GET OUT OF BED every day!
Have you ever heard of or seen a bed sore/pressure ulcer/decubitus wound? Prolonged bed rest causes pressure to build up in specific areas of the body (shoulder blades, tailbone/coccyx, and heels). When the pressure is not decreased or properly managed, a sore develops. Hence, the name PRESSURE UlCER/BED SORE!

The problem with pressure sores is once you see the pressure sore on the surface of the skin, the damage is getting worse under the skin! That’s right…the tissue under the skin is already degrading because pressure sores start under the skin and then work their way to the surface. Nerves, muscles, and even bone can be involved and permanently damaged! There are different stages of a bed/pressure sores based on the depth and degree of tissue involved.
Stages of Pressure Sores |
Signs & Degree of Tissue Involvment |
Pain |
Likely Permanent Damage |
|---|---|---|---|
| Stage 1 | Redness that does not go away when you touch the red area, Warm to the Touch-like the skin has a fever, No broken skin or open wound visible
Tissues Involved: Skin Only |
Can be VERY painful from the nerves involved inside the layers of skin | No |
| Stage 2 | Open wound is visible or skin is broken. Can have a blister-like appearance.
Tissues Involved: Skin + Possible Fatty Layer just under the skin |
Mild to Moderately Painful from nerve endings in the skin | Yes |
| Stage 3 | Visible crater/Open Wound.
Tissues Involved: Skin + Fat layer under the skin |
Possibly Painful–depends on severity of nerve/tissue damage(debrided) | Yes |
| Stage 4 | Open Wound very visible.
Tissue Involved: Skin + Fat+ Muscle + Bone |
Pain Possible but not likely due to severe tissue/nerve damage | Yes |
| Deep Tissue Injury | No OPEN WOUND but the underlying Tissue is Damaged. The depth of tissue involvement is difficult to assess because there is no open wound. The skin is Purple or Dark Red, Soft (Squishy) to the touch, and is either warmer or colder to the touch compared to the surrounding skin. | Painful & Tender to the Touch | Yes |
| Undetermined/Unstagable | Open Wound very visible. Wound bed–what is visible–is covered by a layer of tissue that can be black, gray, brown, have yellow/greenish-yellow puss, and the wound does not fit into the other categories because the depth of the tissue involvement is not clear due to abnormal/discolored layer of tissue masking the base of the wound | Pain Possible but not likely due to severe tissue/nerve damage | Yes |
*Pictures provided by Wikimedia Commons
**Permanent tissue damage can occur with Stage 2, 3, & 4
***Bone infections (osteomyelitis) or sepsis can occur with Stage 4 leading to increased risk of amputation/death
PREVENTION & TREATMENT: Pressure Sores
Below you can view and even purchase heel protectors/pressure sore prevention boots wheelchair cushions for tailbone pressure relief, and bed mobility aids.
You can prevent and treat pressure sores with frequent pressure RELIEF techniques. In bed, turning and using different positions (lying on one side, on the back, and then lying on the other side) every 1.5 to 2 hours with an emphasis on relieving pressure on the bony areas of the shoulder, shoulder blades, hip, coccyx (tailbone), ischial tuberosities (the bony areas just below the cheeks of the glutes/buttocks), and the heels of the feet. When someone sits in a wheelchair, sitting on a BOPPY PILLOW (see picture below) is more comfortable and easily positioned in a wheelchair if a wheelchair cushion is not already in use.
Believe me, the DONUT pillow for coccyx pressure relief is not COMFORTABLE. A BOPPY PILLOW is larger so the surface area is larger resulting in increased distribution of pressure in sitting and overall improved comfort. In the same manner, the BEST position for pressure relief in sitting is leaning forward like you are tying your shoes or positioning the wheelchair in front of the edge of a bed, couch, or recliner, and leaning over the bed, couch, or recliner until the pressure is relieved from the coccyx (tailbone). When decreasing pressure, I recommend leaning forward a minimum of 5 minutes and several times a day if your loved one is sitting in a wheelchair all day.
Go With The Flow…It Does the Body Good
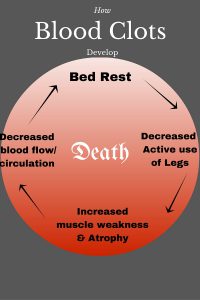
If bed sores are not enough reason to GET OUT of BED, then consider something else that is potentially lethal–BLOOD CLOTS (Deep Vein Thrombosis/DVT). Blood clots can develop when circulation slows down or stops! The veins in our bodies are like a river. When a river is moving fast, it moves debris forcefully downstream. However, if the river flow slows down, the force of water does not clear debris downstream, and debris can build up along the edges. Eventually, the buildup of debris can either stay lodged on the edge of the river (slowing down the flow more) or some of the debris can dislodge along the edges, travel downstream, and make a dam downstream. Either way, the debris disrupts the flow of water! In our blood stream, the debris (aka thrombosis) can be molecules of fat, blood cells, or even air molecules. If the thrombosis dislodges, it can travel (embolize/move) to the heart, lungs, or the brain. When an embolus reaches the heart, lungs or brain, the end result can be sudden DEATH!
Use It or Lose It…Risking Your Secondary Pump
We all agree our heart is a pump–with every contraction-relaxation, blood is pumped/moved throughout the body. In the same manner, the large muscles of the legs are a secondary pump to help the heart move blood from the toes all the way back up to the heart and lungs because the toes are a very long distance from our heart and lungs compared to the head, abdomen, and hands. However, the only way our legs can work as an effective pump is through ACTIVE muscle contraction-relaxation during walking, standing up, transferring, etc… Subsequently, when the legs get weak due to inactivity, increased bed rest, and/or circulation problems (diabetes, cellulitis, congestive heart failure, surgery, etc…), the risk of developing a blood clot increases exponentially! Keeping the legs ACTIVE and STRONG decreases the risk of developing a blood clot because the secondary pump effectively moves blood–inhibiting debris buildup.
So what are the signs of a potential blood clot?
♦ Redness – generally on the back (posterior) side of the leg, soft area behind the knee, or in the calf area
♦ Warmth (fever) – the red area feels warmer than the surrounding skin
♦ Pain/Tenderness – if the clot is in the calf, pain/tenderness occurs with toe raises (the clot is squeezed when the muscle contracts around it).
♦ Swelling/Edema – the leg, ankle, and foot swell due to impeded circulation
♦ Positive Doppler Test – an ultrasound test that assesses the flow of blood for any abnormal flow caused by a clot.
Choking & Aspiration…Not Appropriate Bed Activities
Choking…when food or an object completely blocks the windpipe (trachea) effectively stopping all breathing. What do you do when someone is choking–you administer the Heimlich Maneuver! Okay, now consider trying to successfully administer the Heimlich Maneuver on someone choking IN A BED! Precious seconds are lost as you try to set up yourself and the choking victim in a position for effective delivery of forceful abdominal thrusts.
Aspiration…when food or an object goes down the wrong way–it goes down the windpipe into the lungs instead of down the esophagus into the stomach. Eating while reclined in bed increases both the risk of choking and of aspirating. Both situations can be LIFE THREATENING!
Obviously, daily out of bed activity is very advantageous, but (and there always seems to be a ‘BUT’) you might be struggling with getting someone out of bed after he/she has agreed to GET OUT OF BED. Here is a quick review of the key points covered in the video followed by links for pressure relief equipment, bed mobility aids, and wheelchair cushions.
TIPS for Getting OUT of bed:
1) Bend the knees! A ball rolls better and easier than a board. Bending both of the knees will make rolling easier.
2) Roll him/her on their side and don’t leave anything behind! Make sure he/she reaches toward the edge of the bed with his/her “free” hand and brings the shoulder close to the surface of the bed.
3) Instruct your loved one to, “Look for, find, and keep his/her eyes on the floor.” Usually, we are afraid of what we can’t see and the unknown. By having your loved one keep his/her eyes on the floor, you are boosting their confidence and calming their subconscious fear of falling because they can “see where they are in relation to the floor.”
4) Block his/her bent knees with your body. Your loved one will automatically keep his/her shoulders on the bed; therefore, you need to control the knees so you have control over the “control panel.” If you block the knees, he/she will not FALL OUT OF BED.
5) Keeping the top shoulder forward will “ACTIVATE” the teeter totter–when the legs/feet lower to the ground, the head will raise up!
Tips for Getting IN Bed:
1) Make sure your loved one/client is sitting near the head of the bed (close to the pillow). If he/she sits too low in the bed, they will have to exert unnecessary energy to scoot up toward the pillow once they lie down.
2) Position him/her like they are “side sitting on a horse.” When he/she begins to lie down, side-sitting on the edge of the bed will “ACTIVATE” the teeter totter–when the head/shoulders lower to the surface of the bed, the legs–especially the top leg–will rise up to the surface of the bed.
3) If he/she needs help moving to the center of the bed, I recommend “PULLING” the control panel (hips) toward you with both of their knees bent. REMEMBER: A ball rolls/moves easier than a board. If the legs are straight, you’re trying to move a board!
Take Advantage of Me and My Experience
When I provide images of related products, I am simply showing you some of the options available to address a particular situation. However, if you have friend/relative give you medical equipment and you have a question about how to use, adjust, or set up the equipment, please leave me a comment below and I will make every effort to answer you within 48 hours. I guarantee you are neither the first nor the last person to take on the responsibility of caring for someone that needs medical equipment and are just not sure what to get, how to set it up, or how to use it.
In the same manner, when equipment is delivered, sometimes the representative takes very little time to explain and demonstrate all the features, uses, and adjustments before leaving you with the equipment. To that end, I say, “There is no such thing as a stupid question especially when it is the safety and comfort of you and your loved one hanging in the balance of falls and injuries in the home.”
I encourage you to browse, locate and ask questions before purchasing any medical equipment for the sake of you and your loved one’s safety and sanity.
Related Products
Pressure Relief & Heel Protectors

Oh my goodness! No I have never seen a bed sore, but who would have thought that just not being active can do that! eeakkk.
My gran was very inactive towards the end of her life, old age and immobility, and I wish I had seen this article then. She really struggled to get in and out of bed and would have call for my Mom to do so. Hard on my Mom and hard for her too. It got so much in the end that she rarely got out, and if i remember rightly she died of a blood clot, I wonder if it was caused by this.
I was a teenager at the time, so I don’t remember that much. I wish articles like this had been around then. I hope others can get a real benefit out of it.
Hi Ruth,
Thank you so much for the wonderful comment and for visiting my website. I am sorry to hear about your Grandmother. I truly hope I can help not only the loved ones but also the caregivers.
In regards to blood clots. I was in Physical Therapy school, my first year, and I actually witnessed someone pass away from a blood clot. It was literally instantaneous–one second he was alert and participating with the Occupational Therapist, and the next second he was GONE!!! This happened in a hospital with doctors, nurses, and even a therapist right there. I was terrified. He did not exhibit the signs of having a blood clot, but the autopsy revealed a clot that traveled to the brain and it was lethal. Nonetheless, I learned a lot!
I can only pray I do not have to live through another situation as a Physical Therapist, but there is always a risk.
Thank you again for your story and I wish you the best of health and happiness!
Sincerely,
Shawna PT, MPT
Hi Shawna,
That is mighty scary how quickly bed sore can escalate not to mention how long they take to mend.
Thank you for the tips on getting someone in and out of bed without hurting them or myself.
I have experienced getting specific equipment to help an injured friend and not been shown how to use correctly. I appreciate your offer of experience and knowledge, the related products you shared with us and your medical equipment page. 🙂
Hello Helen,
Thank you for visiting my site. Bed sores are very scary and the recovery is painful as well as long and drawn out because so many things are working against the healing process. It is always a pleasure to know I have helped at least one person and through this website I am striving to help as many caregivers as possible.
Most patients initially do not like the term “Physical Therapy” but through planning, targeted interventions, education and determination, they meet their goals and then HATE to see the home therapy come to an end.
At least here, I don’t have to say ‘Goodbye’ and now all of my patients have a way of communicating with me even after they no longer need home-based therapy.
I hope you and those special loved ones in your life never need Physical Therapy, but if they do, I am here to help. Thank you again for your time and I wish you and your loved ones optimal health and happiness.
Sincerely,
Shawna